Is Ontario’s critical care system prepared for a surge in cases?
The Covid-19 pandemic has presented challenges for Ontario’s critical care system. As infections trend upward, the scientific community cautions that hospital admissions will likely climb in the weeks to come.
On December 6, the Ministry of Health reported 168 patients in the province’s Intensive Care Units (ICU) due to Covid-related critical illness. That is the highest number of Covid-related ICU patients in more than two months, when the number reached 171 Covid ICU patients on September 30.
Ontario’s Covid-19 Science Advisory Table indicated that ICU occupancy is projected to climb and may reach 200 patients by the new year. While researchers continue to study the new variant Omicron, questions remain over its transmissibility and the severity of the disease. What we know so far is the impact of the pandemic on the health care system prior to the latest variant detected in Canada more than one week ago.
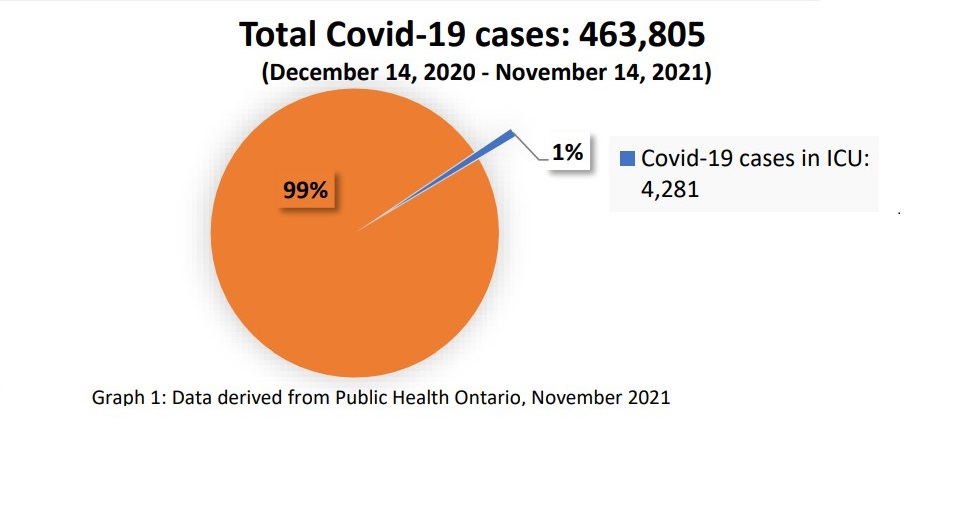
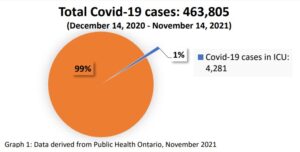
According to a comprehensive report, the Confirmed cases of Covid-19 following vaccination in Ontario, by Public Health Ontario, data collected between December 14, 2020 and November 14, 2021, show that 463,805 people tested positive for Covid-19. In that one-year period, 22,009 people were hospitalized. That represents five percent of all infections in that time frame.
Due to worsening complications from the virus, a total of 4,281 hospitalized patients required further medical intervention and were admitted to the ICU. That represents one percent of all infections during that one-year period. (see graph 1, above)
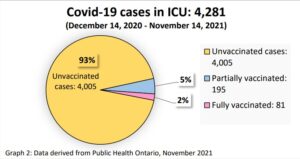
The medical community continues to advise that Covid-19 vaccines play a critical role in reducing instances of hospitalization and helps prevent against severe outcomes. In the one-year time frame following the first administered does of the Covid-19 vaccine, 195 partially vaccinated patients were admitted in the ICU due to Covid-related critical illness. In the case of those who were fully vaccinated, that number drops to 81 patients in the ICU. (See graph 2)
When further broken down by age group, ICU patients aged 80 years and older, the report indicates that 60 were partially vaccinated compared to the 343 who were unvaccinated. That number drops to 22 for those who were fully immunized. (See graph 3)
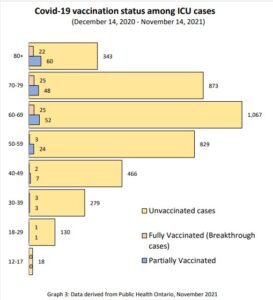
The greatest number of ICU admissions were of unvaccinated people in their 60s : 1,067 patients with confirmed Covid-19 infection. In the case of those who were partially vaccinated, 52 Covid-patients were admitted to the ICU, compared to just 25 who were fully vaccinated.
The numbers are far fewer in the age group from 18 to 29. Only one ICU patient was fully vaccinated, another only partially vaccinated. During the year, a total of 130 unvaccinated patients in that age group were admitted to the ICU.
Medical officials maintain that seniors and individuals with pre-existing medical conditions are often considered more vulnerable to severe infection due to weakened immune systems and age-related complications. On the basis of data collected over the year, the Report suggest that “there is evidence that vaccines reduce symptomatic infection, the severity of illness as well as transmission”, when Covid-19 cases occur following vaccination.
It will take time to fully understand the impact of the new variant on the critical care system. In the meantime, the next part of this series will examine the data on the severity of outcomes in Covid-19 cases post immunization.