Heightened public health concerns as Omicron is on the move
Health officials are raising the alarm as the Covid-19 variant Omicron has more than thirty mutations. Researchers are suggesting it is spreading twice as fast as the Delta variant.
Some medical experts theorize that Omicron has picked up genetic material from other viruses that cause the common cold, potentially making this strain more transmissible. While many unknowns remain with the new variant, people’s fears and anxieties have grown over the severity of accompanying illness and how lethal Omicron may be.
Others fear that a surge in infections may put additional strain on the healthcare system. The added pressures have spilled over to health care staff who have been treating patients through successive “Covid waves”.
Ontario’s Science Table cautions that the province’s critical care system “does not currently have capacity to accommodate a surge as it did during waves 2 and 3.” Scientists attribute this to “worsening staffing shortages, healthcare worker burnout and health system recovery efforts”.
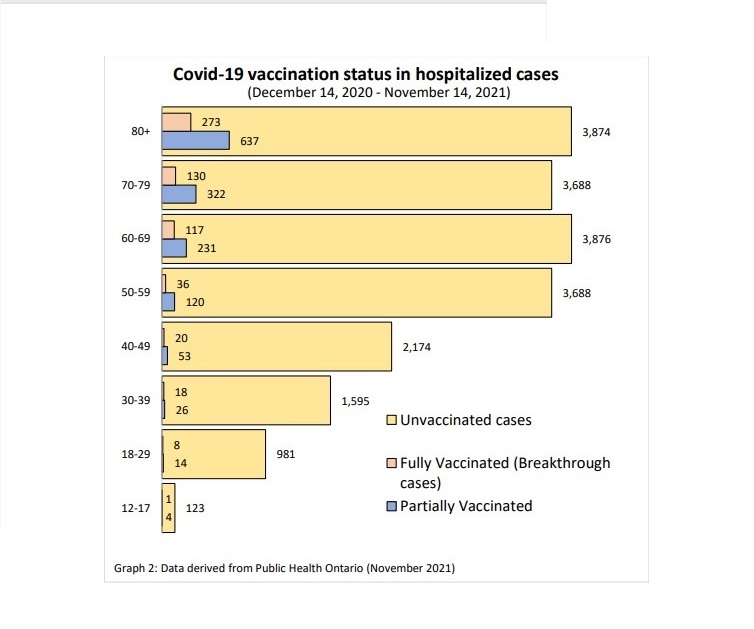
In the meantime, health officials emphasize the importance of vaccination against Covid-19 to reduce the risk of severe outcomes. According to a comprehensive report, the Confirmed cases of Covid-19 following vaccination in Ontario, from Public Health Ontario, data collected between December 14, 2020 and November 14, 2021, show a total of 22,009 Covid-19 cases which required hospitalization over that one-year period, (see graph 1, above).
Of those patients in hospital due to Covid-19 infection, the majority, 91%, were unvaccinated. Six percent of patients (1,407), were partially vaccinated, having completed one dose of a two-dose vaccine. When considering the 603 fully vaccinated patients who required hospitalization, that figure drops to just 3% off all Covid-19 hospitalized patients.
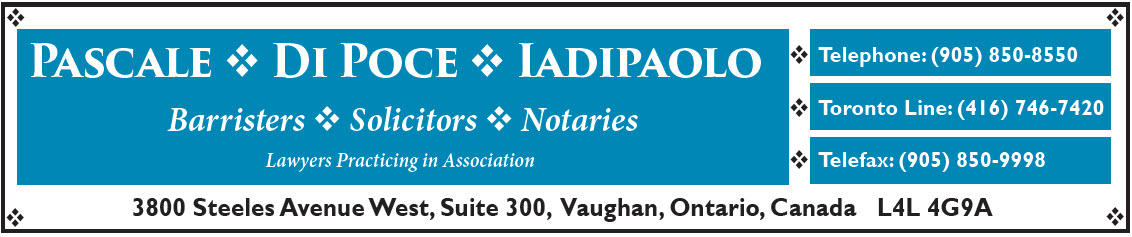
In the early phase of the vaccine roll-out, seniors aged 80 and over were prioritized for immunization. Health experts consider people in that age group more vulnerable. Usually, they have weaker immune systems and often exhibit pre-existing medical conditions, which can make them more susceptible to severe infection requiring hospitalization.
For instance, in that one year, more than 3,800 unvaccinated seniors over the age of 80 required hospital intervention, (see graph 2, below). In the case of those who were partially vaccinated, that number plummets to 637 cases which required hospitalization. That number drops to 237 seniors in the same age group who were fully vaccinated and in hospital due to Covid-19.
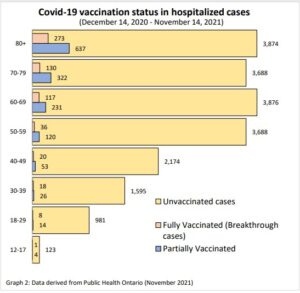
As the age of younger people become infected with Covid-19, the number of hospitalized patients who have at least one dose of the vaccine appears to decrease significantly as well. For example, about the same number of unvaccinated people in their sixties as those over the age of eighty required hospitalization after contracting the virus. However, only 231 partially vaccinated patients in their 60’s required hospitalization, compared to just 117 who were considered fully vaccinated.
The numbers continue to fall among the vaccinated as the age of patients hospitalized with Covid-19 decrease.
The next series will take a closer look at the vaccination status among hospitalized Covid patients with data detailing the severity of infection and how many end up in the ICU.